© 2024 Embrace Hospice and Home Health
All Rights Reserved
All Rights Reserved
We don’t often think about the importance of staying hydrated. We may go for hours and hours without a sip. We may wait until we’re thirsty to get a drink.
Generally, you should drink ⅓ of your weight (in pounds) in ounces of water daily. For example, if you weigh 150 pounds, drink 50 ounces of water (or other hydrating beverages) daily.
Many health problems and medications can affect the amount of water we need, so it’s best to talk with your doctor about your specific needs.

As we get older, our ability to regulate the amount of water in our body declines. What’s more, our lifestyle and habits may change over time. We may have been more active, naturally drinking more water. But now we don’t exercise as much or at high intensity.
We may have commuted to work every day with a drink in the cup holder. We sat at our desks with a tumbler of water within reach, a constant reminder to take a drink.
For seniors, we need to maintain a 55% level of water in our bodies. Dehydration, even in mild cases, can harm health and exacerbate existing medical conditions. Symptoms like confusion, dizziness, fatigue, joint pain and constipation can result from inadequate hydration.
The importance of staying hydrated extends beyond everyday life for seniors. It becomes even more critical when recovering from an illness, injury, or medical procedure. During these times, the body requires additional support to heal and regain strength and adequate hydration plays a vital role.
Some of the ways hydration helps you heal include:

Many of us take multiple medications, some of which may cause an increase in urination. What’s more, many chronic health conditions, like diabetes and kidney disease, can contribute to this loss of fluids. Losing too much fluid is even more dangerous in summer.
During the hotter months, the combination of higher temperatures and perspiration can lead to a greater risk of dehydration. Heat-related illnesses like heat exhaustion and heat stroke are also more common in seniors and can be life-threatening.
Look for shade, go into an air-conditioned building, and avoid prolonged exposure to heat and sun when temperatures and humidity rise.
Drinking enough water isn’t the only way to prevent dehydration. Other hydrating beverages and foods are also options.
Foods like fruits and vegetables with high water content can help also us stay hydrated: strawberries, tomatoes, watermelon, celery, and cucumbers. Beverages like herbal teas can increase hydration too. But it’s essential to limit caffeine and alcohol. They can have a diuretic effect.
Remember that staying hydrated is important at any age but is critical for seniors. Staying hydrated gives our bodies the necessary support to heal, manage medications, boost immune function and regain energy and mobility. Be sure to talk with your doctor about their hydration recommendations for your needs.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2908954/
https://www.ncoa.org/article/how-to-stay-hydrated-for-better-health
Watching someone you love suffer from Alzheimer’s or another memory debilitating illness is incredibly difficult, and it can be even more challenging to decide when it’s time to consider hospice care. Here, we are sharing five signs it may be the right time to consider the extra support of hospice care for an Alzheimer’s patient.
The Functional Assessment Staging (FAST) Scale is a tool used to determine if changes in a patient’s condition are related to Alzheimer’s disease or another condition. If due to Alzheimer’s, the changes will occur in sequential order. Alzheimer’s disease-related changes do not skip FAST stages.
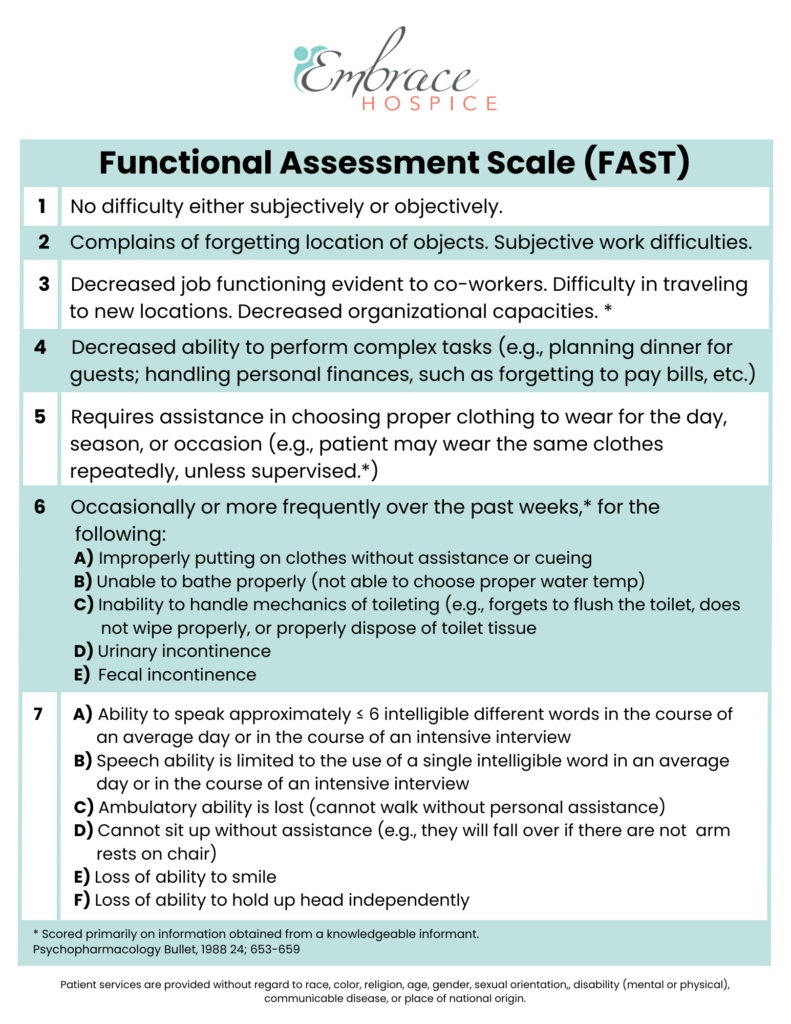
This means a person is no longer able to get around on their own. For example, they require assistance getting from room to room.
Without assistance, you may notice they put their shoes on the wrong feet or their day-time ‘street’ clothes on over their pajamas. They are also unable to bathe without assistance.
This includes urinary or fecal incontinence or both.
This may begin as the patient only saying 5-6 words per day and gradually reduce to only speaking one word clearly until they can no longer speak or communicate at all. This will also include the inability to smile.

Hospice care is for patients with a life limiting illness and a life expectancy of six months or less. The main focus is to manage pain and symptoms and ultimately keep the patient comfortable. When you choose hospice for your loved one, their care team can help you to understand what to expect in the final stages of Alzheimer’s. They will also provide support to you and the rest of your family throughout the end-of-life process.
If you would like more information on hospice care for Alzheimer’s patients, please contact us. We are here to answer any questions you may have.
This May, join us in celebration of America’s 4.4 million registered nurses who make a touching difference in the lives of patients and their families. Exceptional nurses often have a true passion for helping others, backed by compassion and empathy.
In honor of this month, we express our appreciation for home health nurses, hospice nurses, and nurses who work in the skilled nursing facilities that partner with us as hospice and home health providers.
Nurses make a profound impact in improving the quality of life of individuals in skilled nursing facilities, hospice care, and home health care. We invite social workers, medical professionals, and anyone who has been touched by a nurse to celebrate Nurse Appreciation Month with us. This is your reminder to thank your nurses and show you appreciate their “special touch”.

Nurses working in skilled nursing facilities serve a vital role in helping individuals get back on their feet after an injury or illness. While in rehabilitative nursing care, patients are supported by nurses who are committed to helping them improve their quality of life and regain strength during recovery.
Often, it is because of the support from nurses in rehabilitative nursing care that individuals can safely return to their homes for ongoing support from home health nurses. This allows individuals to continue recovering from the comfort of their own homes.
Throughout the month of May, we also recognize and show we appreciate the exceptional home health nurses that support patients in their homes. Home health nurses play a vital role in supporting an individual’s road to recovery as they strive to regain independence and autonomy in the home. Home health staff support the holistic health of individuals beyond physical care by also providing social and emotional support.
Hospice nurses have a special role in the lives of patients diagnosed with a terminal illness and their families. Nurses providing end-of-life care through hospice services help reduce unnecessary pain and suffering, making individuals as comfortable as possible in their final months or days of life. In addition, hospice nurses generously share their skills and compassion to provide supportive care that improves an individual’s quality of life, developing strong bonds with patients and their families.

Often, hospice nurses go above and beyond the call of duty, showing exceptional compassion for those nearing the end of their life. Not only do hospice nurses support an individual’s wishes, but they also provide support resources for family and friends during difficult times. Most families never forget the lasting impact the nurses made during an incredibly challenging period in their life.
Nurses in skilled nursing facilities, hospice care, and home health nurses demonstrate admirable qualities such as compassion, patience, and empathy. On behalf of our team and our partners, we honor the champions that have dedicated their careers to improving the lives of others. We couldn’t do it without you!
Some older adults and people with serious illnesses, unfortunately, experience the end of life in certain healthcare settings that do not align with their desired wishes. If you have a serious illness or are a caregiver of someone planning end-of-life care, knowing the difference between palliative care and hospice care can help you make an informed decision when the time comes to transition to one of these healthcare settings.
Palliative care is a form of care that focuses on improving your quality of life and that of your family when you are living with a serious illness. It focuses on your whole-person health rather than only on your condition. If you are receiving palliative care, your treatment plan may focus on reducing symptoms of your illness and on improving secondary conditions such as depression, sleep deprivation, and side effects of medications.
Palliative care may be given in various healthcare settings, such as at the hospital, a residential care facility, or your home. Anyone can receive this type of care regardless of age or the severity of their condition.
If you receive palliative care, you may work with and be treated by various healthcare professionals, including doctors, nurses, social workers, pharmacists, physical therapists, counselors, and nutritionists. If you need spiritual care, your palliative care team may even include a chaplain. The healthcare professionals that make up your palliative care team will depend mainly on your recovery needs and level of care.
Studies show that palliative care offers many benefits, including:

Hospice care focuses on improving your comfort and quality of life when you are nearing the end of your life. This type of care is usually given in circumstances in which an illness continues to progress despite treatment or when the patient chooses not to receive certain treatments. Hospice care is similar to palliative care in that it provides comfort care and support for the family. However, treatments are not given to improve the illness.
Like palliative care, hospice care can be given in many different healthcare settings, though it is most frequently given at your home, where you can be most comfortable and spend quality time with your loved ones. In addition, it is typically given when your healthcare provider believes you have no more than six months to live. Some benefits of hospice care include 24/7 access to nurses and healthcare workers who can address and relieve symptoms and side effects and access to medical equipment and medications that can reduce your discomfort.
Many of the same types of healthcare professionals that make up a palliative care team will also be part of your hospice care team. This includes doctors, nurses, social workers, chaplains, and volunteers who dedicate their time to giving you the support you need and making you feel as comfortable as possible during your final months.
To be eligible for hospice care, you will discontinue aggressive treatment efforts to combat your terminal illness (such as experimental surgeries, aggressive chemotherapy, or other treatments that require prolonged hospitalization and recovery). However, you may continue to receive treatments for other conditions, such as antidepressants to treat depression or insulin medicines to control Diabetes.
Comfort care and end-of-life care are both terms that describe the type of care you receive when you are near the end of your life and are no longer receiving treatment for your illness. It is highly similar to palliative care in providing you with whole-person care that focuses on your physical, social, emotional, and spiritual health. Comfort care and end-of-life care may include palliative care or hospice care, or a combination of both.
Sometimes, palliative care is given as part of hospice care, and both types share many similarities. For instance, the goal of both palliative and hospice care is to improve your quality of life and help you find relief from painful and severe symptoms and side effects of treatment. Both types of care also focus on whole-person health. However, there remain many differences between palliative care and hospice care.
Some of these differences are:

You may want to consider palliative care if you or your loved one has a serious illness or chronic condition that requires long, intensive care or that causes severe physical symptoms and/or emotional distress. For example, cancer, heart disease, AIDS, and kidney failure are some of the many conditions that can benefit from palliative care.
Additionally, palliative care may benefit you if you:
A person may transition from palliative care to hospice care if their doctor thinks they have no longer than six months to live. Sometimes, it can be difficult for doctors to predict exactly how long it will take for a particular disease to run its course or how long a person has left to live if their health is in decline. In these circumstances, it’s important to consider how transitioning to hospice care could improve your quality of life during your final months.
According to the National Library of Medicine (NLM), doctors should strongly consider referring chronically ill patients to hospice care if they spend more than half their time in bed, are unable to function efficiently, and are experiencing both physical and psychological distress. The NLM adds that hospice referrals are usually necessary when the patient’s condition has progressively declined to the point that their highest priority is to take control of their healthcare and achieve the greatest possible comfort in their homes as they near the end of life.
Talk to your doctor if you think you may need hospice care but aren’t sure when you should transition out of palliative care. Your doctor can talk to you at length about your options and the benefits of transitioning to hospice care based on your condition and unique circumstances.
Taking advantage of hospice care as soon as it’s needed could result in access to quality care and lots of extra quality time to spend with your loved ones. Additionally, studies show that patients who plan their care in advance are more likely to be satisfied with their care, given how they can make decisions that align with their end-of-life wishes.
Consult with your healthcare provider if you or your loved one is interested in learning more about palliative care or hospice care. Your doctor can refer you to a palliative or hospice care specialist who can answer all your questions and help you determine which of these services may be more ideal.
Palliative care and hospice care are covered by many major health insurance providers, including Medicare. The exact benefits covered will vary based on your health plan. Benefits covered may include medical equipment and supplies, skilled nursing care, bereavement support, and medications to provide comfort, among many others.
Hospice At Your Side has resources for home health and hospice services throughout the United States. Specialty services we offer include diabetes care, orthopedics, and pain management. Call us today to learn more about our many home healthcare services.

It’s time to speak up about breast cancer, and the month of October is dedicated to doing just that. As the most common form of cancer, it’s likely that someone in your life whom you care for deeply has been diagnosed with breast cancer. Given how prevalent breast cancer is and the repercussions it has on individuals and families affected, this month is a time to rally together and raise awareness about it.

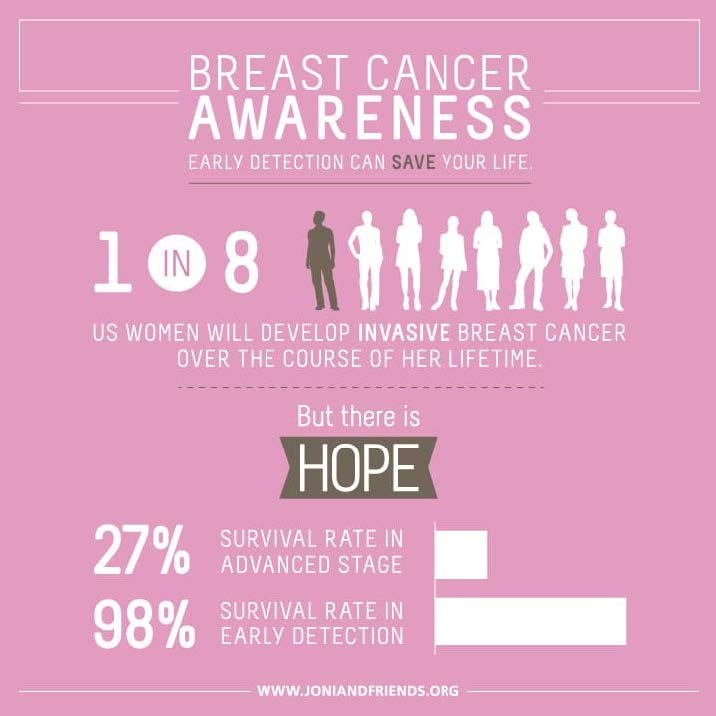
In the United States, more women die from breast cancer every year than any other form of cancer. It’s currently estimated that 1 in 8 women in their lifetime will be diagnosed with an invasive form of breast cancer. Two of the greatest risk factors of getting breast cancer are female gender and older age, though men and younger women can get it as well. The statistics are alarming, and a diagnosis can feel daunting and isolating, whether it’s yourself or a loved one or family member who is receiving it. Fortunately, breast cancer research continues to thrive, which has led to improvements in screening processes and treatment success. These improvements have been given some of the credit for the slightly decreased death rate from breast cancer over the past several years. In order to take further advantage of the strides we’ve made in battling breast cancer, we must continue to educate our communities about the screenings and treatments available.
While there is no way to guarantee prevention of breast cancer, it is recommended that all adult women perform a breast self-exam monthly. This is a great way to self-monitor for any changes or abnormalities that may occur in the breast tissue. As you age, this becomes an even more important habit as age is one of the main risk factors. It is important to note that not every growth or lump felt in the breast tissue is a cancerous mass. Some non-cancerous masses are abnormal but do not grow outside of the breast tissue. While these lumps do not innately pose a risk, some of these growths can increase a women’s risk of getting breast cancer down the road. Any abnormality or change in your breast tissue that you notice or feel should be examined by a health professional immediately. Just under half of women diagnosed with breast cancer were diagnosed after noticing a lump during a self-exam, so the importance of this routine cannot be overlooked. In addition to regular self-exams, maintaining a healthy weight through exercise and a nutritious diet is another important way to reduce your risk of breast and other cancers.
Should you receive a diagnosis of breast cancer, take the time to find a team of doctors whom you are comfortable with and trust with your care. This team can include an oncologist, or cancer doctor, a surgical oncologist, a radiologist, a case worker, a registered dietician who specializes in cancer nutrition and possibly several other specialty providers. These individuals will be with you, alongside your personal support system, to make sure you receive the best care available from diagnosis on. Treatments and interventions will differ depending on the type of breast cancer you are diagnosed with and your doctors will help you navigate all of the options and should use their expertise to recommend the best course of action. Make sure you feel comfortable asking questions and engaging in your treatment plan. Your providers have the knowledge and the skill sets to provide excellent care, but it is just as important that you feel included in the decisions being made and prepared for the treatment road ahead.

Whether you are young, old, male, female, part of a high-risk category or not, it is our shared efforts in spreading awareness this month of October and all months following that will successfully raise awareness, education, and resources about breast cancer to every individual diagnosed and every family and friend supporting them. As a society working together, it is within our reach to decrease breast cancer diagnoses within our communities and to improve the outcomes and survival rates of those diagnosed.
National Breast Cancer Foundation, INC.
As a survivor of breast cancer, few will understand the struggle you endured, but many acknowledge and honor the strength it took to carry on.

Alongside the relief and celebration that comes with completing treatment and hearing the long-awaited word “remission” may come a host of other emotions. Some of them may not be as positive. You may feel fear of the cancer coming back or anxiety about not seeing your treatment team as often. Surgeries and treatments can alter the way you feel about your body. These emotions are natural after what you’ve been through, and it’s important to know that you’re not alone and that you have resources at your disposal to live your life as fully as possible following recovery.
After completing treatment and entering into recovery, it is important to abide by your doctor’s recommended follow up care. This care often includes checkups every few months for the first several years after treatment. As your cancer-free time increases, the frequency of appointments can begin to decrease. If you had breast-conserving surgery to include a lumpectomy or a partial mastectomy, it is recommended that you get a mammogram 6-12 months after surgery and radiation and continue to get them annually for monitoring. Pelvic exams may also be included in your follow up care as some of the hormone drugs can increase your risk of endometrial or uterine cancer. Another test that may be done, especially if you have gone through menopause, is a bone density scan. Monitoring your bone health will be a priority for your doctor especially if your cancer treatment included drugs that can reduce bone density.

Battling cancer and enduring the challenges that come with treatment can leave you feeling exhausted. It can be challenging to find the energy to keep up with follow up care, knowing that it will be a crucial part of your life as a survivor. Express any concerns or anxiety or overwhelm you are feeling about your continued treatment and monitoring with your doctor. Collaborate with them and let them help you feel more in control when it comes to your checkups. Equally important as your medical team is your support system. Continue to lean on the individuals who supported you through treatment, whether it be family, friends, a loved one, a support group or a therapist. Support systems can often help to shoulder some of the burden when it comes to remembering appointments, driving to procedures, and encouraging you to continue doing the things you love outside of your healthcare.

Every single individual’s experience with surviving breast cancer is unique and special. You will have your own thoughts, feelings, challenges and success that you overcame and that you will continue to experience as you embrace a heightened awareness of your health for the rest of your life. Beyond this, you are an example of hope and strength for others who are fighting their own battle against breast cancer. Continue to spread awareness this month and every other so that we can continue to win more of these battles.
Everyone knows about heart attacks… but have you ever heard of atrial fibrillation? Despite being the most common heart arrhythmia (meaning irregular heartbeat) that is medically treated and being the cause for 1 in 7 strokes, most people aren’t familiar with atrial fibrillation. Surveys have revealed that even those who are aware of it often don’t consider it a serious medical condition. Education is key here, as leaving atrial fibrillation untreated doubles the risk of heart-related deaths and increases the risk of having a stroke significantly. It is estimated that by 2030, about 12.1 million people living in America will have a diagnosis of AFib. Considering how high that number is, it’s time to start paying attention to what it is and how you can mitigate yours and your loved ones’ risk factors!
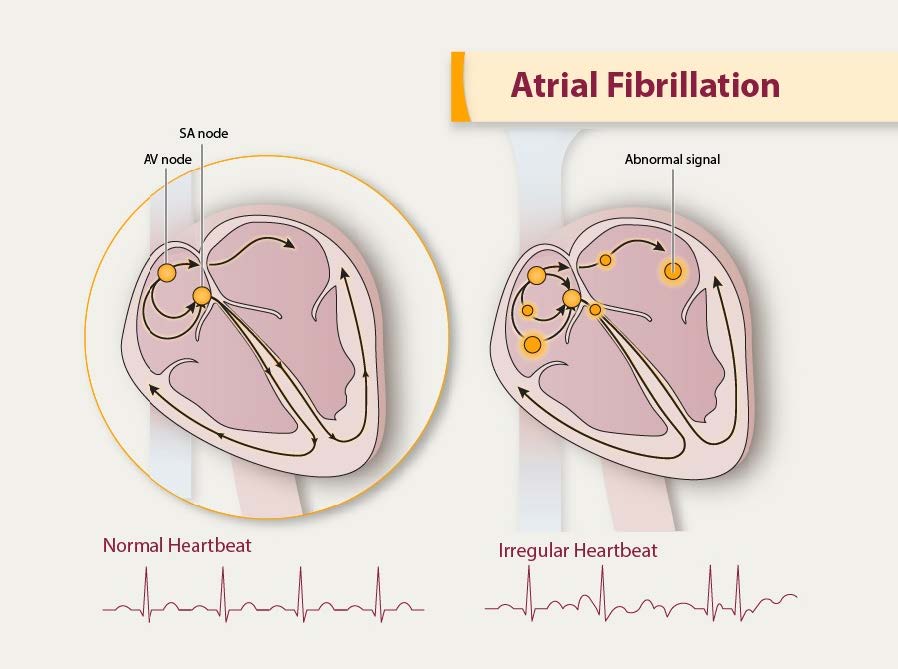
So what is atrial fibrillation? Atrial fibrillation, abbreviated AFib, is an abnormal heart rhythm during which the top chambers of your heart, called your atria, quiver rather than beat, leading to inefficient movement of blood through your heart. Given the inefficient contraction of the heart, individuals with AFib are at a higher risk for clots. The higher risk of clotting and the decreased ability of the heart to pump blood efficiently is what leads to an increased risk of further heart conditions and stroke should a clot form and travel to the brain.
While some individuals with AFib might not know they have it and may experience no symptoms at all, others could experience a number of various symptoms. Pay attention to the symptoms and take action. Consider scheduling an appointment with your doctor if you or a loved one are experiencing any of the following:
In addition to symptom monitoring, there are a number of risk factors to be aware of related to AFib. Considering the risk of stroke and heart disease increases significantly with AFib, mitigating the risk factors of AFib is crucial. Risk factors include:
If any of these risk factors apply to you or a loved one, consider if your risk factors are modifiable, meaning you have more control over reducing how much of a risk they pose. Focus on lowering your blood pressure, losing weight if appropriate, reducing or eliminating alcohol intake and quitting smoking. Consuming whole, natural foods when possible, incorporating exercise and purposeful movement every day, and staying hydrated can go a long way in preserving your health!
If you have already been diagnosed with AFib, it is important to continue to mitigate as many risk factors as you can using the guidance above, in addition to seeking proper medical treatment for your condition. Lifestyle changes, even after being diagnosed with AFib, can greatly decrease the severity and frequency of your symptoms. These lifestyle changes include cutting back on alcohol, reducing caffeine, quitting smoking, exercising regularly, eating a nutrient rich diet, losing weight if required and lowering your blood pressure. When prescribed medications for AFib, especially blood thinners to reduce the risk of clots, it is imperative that you follow the guidance of your doctor and stay consistent with the treatment.
Given that AFib is a chronic condition, meaning it doesn’t go away, it is likely that you will be on medication to manage it for the rest of your life. This can be scary and anxiety inducing if you don’t understand your medications or don’t have a plan to stay on track. Meet with your doctor and be sure to understand what medications you are taking, why you are taking them, how long you will be taking them for and what side effects to look out for. You deserve to understand and feel comfortable with your treatment, so be sure to collaborate with your medical team and find support from your loved ones.
Atrial fibrillation – if it’s not taken seriously, it could cause serious problems!
Know the symptoms, schedule regular visits with your doctors, and practice a healthy lifestyle to reduce your risk!
Image 1 – https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
Image 2 – https://www.mcrmedical.com/blog/aha-2020-guidelines/
Heart Foundation –
https://www.heartfoundation.org.nz/your-heart/hearthelp/atrial-fibrillation/managing-your-af
CDC – https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
American Heart Association –https://www.heart.org/en/health-topics/atrial-fibrillation/what-is-atrial-fibrillation-afib-or-af
When you hear the word “diabetes”, chances are it hits home on some level. It may be a loved one, a parent, a friend, or yourself who is living with this disease. They are just one of 34 million Americans living with a diabetes diagnosis. Another 96 million have prediabetes. Of those 96 million, 80% of them do not know they have prediabetes, highly increasing the likelihood of developing diabetes down the road. The consequences of this disease are high, and the prevalence across our population is increasing. November is American Diabetes Month, a month dedicated to raising awareness about how to prevent diabetes and improving the resources available to those living with it.

There are three different types of diabetes that contribute the most to the diabetes epidemic. They include prediabetes, type 1 diabetes, and type 2 diabetes. Though they are all a bit different from one another, all forms of diabetes are related to insulin and blood sugar levels. Insulin is a hormone released by the pancreas and its job is to regulate the levels of glucose, also known as sugar, in your bloodstream.
Type 1 diabetes, also known as “insulin dependent” diabetes, is an autoimmune disorder during which the cells of the pancreas that produce insulin are destroyed. When these cells are destroyed, the body cannot produce insulin. This results in glucose staying in the bloodstream rather than being taken up by the cells in your body. Over time, this causes blood sugar levels to rise without the body having a way to naturally regulate them back down to normal. Individuals with type 1 diabetes are often diagnosed during childhood or adolescence, though it is possible for adults to develop type 1 diabetes. The treatment for type 1 diabetes must involve taking insulin every day because the body cannot make it and checking blood sugar levels regularly throughout the day. Consuming a healthy, balanced diet and partaking in regular exercise should be included in the management of type 1 diabetes to help avoid complications.
Type 2 diabetes, also known as “insulin resistant” diabetes, is caused by the body not producing sufficient amounts of insulin or the body resisting the insulin being produced. In both cases, the body is unable to properly regulate blood sugar levels. The biggest risk factors for developing type 2 diabetes are obesity and high blood pressure. In the past, you would see this type develop most often in adults over 45. In recent years, the number of children and teens developing type 2 diabetes has been increasing as a result of poor nutrition and rise in obesity. Due to the nature of type 2 diabetes, it can be successfully managed through a healthy diet, regular exercise, and maintaining a healthy weight. In some cases, when lifestyle changes aren’t sufficient, type 2 diabetics must supplement with oral medications and insulin to help control blood sugar levels.
When blood sugar levels are higher than normal but not high enough to be classified as diabetes, it is called prediabetes. While prediabetes isn’t technically classified as diabetes, it often develops into a full diagnosis of diabetes if no intervention is implemented. Awareness is the key to success here as many individuals may not develop symptoms until it is too late. Lifestyle changes that are implemented by individuals with prediabetes can often prevent or drastically delay the development of type 2 diabetes. These lifestyle changes include following a diet of minimally processed foods and regularly partaking in exercise.
If you or a loved one have already been diagnosed with diabetes or you suspect you may be at risk, schedule an appointment with your doctor to share your concerns and maintain regular checkups. Without proper care, serious complications such as hypoglycemia (low blood sugar), kidney failure and heart disease can occur. Preventing these complications requires adherence to treatment per your doctors’ guidelines, a healthy diet and regular exercise.
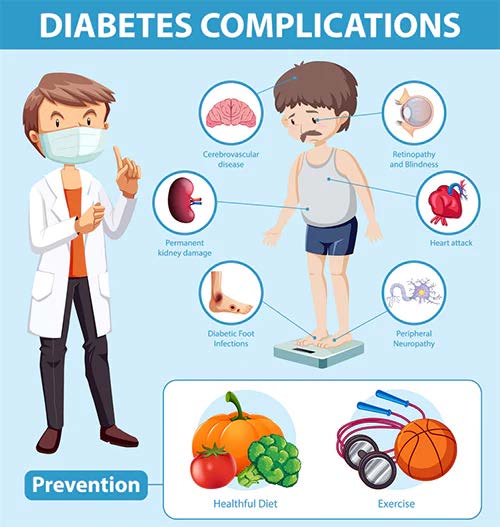
Diabetes is widespread across America, but it is not an insignificant diagnosis. This disease must be taken seriously and treated properly in order to avoid complications. Unfortunately, not everyone has equal access to the medical resources and education that makes living a normal and fulfilling life with diabetes possible. Raising awareness and equalizing care is one of the major goals throughout the month of November. We encourage you to take the time this month to share this article with family, friends and loved ones. Encourage those around you to speak up about the risk and prevalence of diabetes in our communities. The more we open up the discussion about diabetes, the more we can band together in order to support our loved ones and improve the health of our community.
Visit The American Diabetes Association to learn more or to offer a donation towards ending diabetes. https://diabetes.org/
Image 1 – https://newatlas.com/medical/type-2-diabetes-protein-beta-cell-protection/
Image 2 – https://www.diabeticwarehouse.org/blogs/articles/diabetes-complications
American Diabetes Association – https://diabetes.org/
CDC – https://www.cdc.gov/diabetes/library/spotlights/diabetes-facts-stats.html
Endocrine Society –
https://www.endocrine.org/patient-engagement/endocrine-library/diabetes-and-older-adults
National Institute on Aging – https://www.nia.nih.gov/health/diabetes-older-people
Speare Memorial Hospital –
https://spearehospital.com/november-is-american-diabetes-month/# World Health Organization – https://www.who.int/news-room/fact-sheets/detail/diabetes

We all grieve differently, but one thing remains true for everyone: the importance of taking care of yourself. Whether you’ve found yourself in a state of just going through the motions or you’ve put all your focus on taking care of your loved ones, it can be easy to put your own needs on the back burner when facing the loss of a loved one.
However, it’s absolutely imperative that you take time to focus on yourself, too. In honor of Mental Health Awareness Month, we are discussing the importance of self-care throughout the grieving process.
Mental Health Awareness Month dates all the way back to 1949 when the National Association for Mental Health (now known as Mental Health America) first organized the observance in the month of May to help raise awareness and lessen the stigma attached to mental illness.
For a long time, society looked at mental illness as being just one thing. There was always a negative stigma attached to the term, and people often thought of those living with a mental illness as having ‘gone mad’. However, that is simply not true. Over time, we’ve learned more about the many layers and types of mental illness.
Mental illness is the term used to describe mental health conditions that impact a person’s mood, thinking, and behavior. Common mental illnesses include:
Losing a loved one can be a traumatic experience. You may feel as though you lost a part of yourself and that your life will never be the same. While there is some truth to this, it’s important to remember that you are still here and must go on living your life.
“We don’t move on from grief. We move forward with it.”
– Nora McInerny
Feelings of sadness, anger, loneliness, and hopelessness are all common throughout the grieving process. However, these feelings can sometimes develop into chronic grief which can in turn become a mental illness. In some cases, grief can lead to depression.
Symptoms of chronic grief can include:
Self-care used to be thought of as bubble baths and pampering yourself, but there is much more to self-care. Just like the grieving process, self-care can look different for everyone. But the overall concept is to take care of yourself physically, mentally, and emotionally.
To take care of yourself physically is pretty simple: eat a well-balanced diet, drink plenty of water, exercise regularly, and practice healthy hygiene habits. However, taking care of yourself mentally is a little less cut and dry. This is where it really differs from person to person. To take care of yourself mentally and emotionally, you need to take time to do the things that make you feel good and happy. Hobbies are a good place to start when focusing on taking care of yourself mentally. Maybe you enjoy sitting outside and reading a good book, maybe you are an artist, maybe you enjoy taking long walks with your dog. Whatever it is that leaves you feeling happy and fulfilled, do it!
Research shows the more you practice self-care, the more confident, creative, and productive you are. This also leads to experiencing more joy, making better decisions, building stronger relationships, and communicating more effectively. Overall, you will be in a better frame of mind, making you a better version of yourself. This is not only good for you, but it’s also good for those who depend on you.
When you take time to take care of your whole self (physically, mentally, and emotionally), it will help you to process your feelings of grief in a healthier way.
Always remember that you do not have to face the journey of grief alone. Lean on friends and family to help you through. Don’t be afraid to talk about your feelings. Sometimes we feel the need to be strong for those around us. If this is the case and you would feel more comfortable talking to someone outside the family, lean on the support of your hospice bereavement team. Our kind, compassionate bereavement coordinators are always available to talk or just listen. Never hesitate to reach out.
If you or someone you love is struggling with their feelings of grief and would like to talk to one of our bereavement coordinators, please contact us at 1-800-695-7074.

By: Anonymous
May is Asian American and Pacific Islander (AAPI) Month, a time to learn about and celebrate the rich histories and cultures of Americans from the Asian continent and the Pacific Islands. The AAPI population is remarkably diverse, with 24 million people tracing their roots to over 30 countries. Many different cultures mean many different beliefs and traditions regarding the passage from life to death.
Demographic research reveals that AAPI Americans are less likely to access hospice and palliative care than other groups. Asian Americans, for example, have been shown to use fewer end-of-life services. Studies attribute this to cultural beliefs, language barriers, attitudes about death, and family-centered decision-making. But good hospice and home care can meet these challenges.
We recognize that the AAPI community has diverse attitudes and practices surrounding illness, hospice, and death.
Although some AAPI practices are widely shared, such as respecting elders, using white and yellow colors, and burning incense, some practices vary. Chinese and Korean values can require the family to keep vigil by a dying loved one. The Chinese tradition, however, may maintain a hierarchy within the family structure, while the Korean tradition might maintain the division of genders. In other AAPI traditions, individuals, like expectant mothers, are discouraged from visiting someone at their end-stage of life for their own protection. In addition, some cultures place great value on a loved one being cared for in their own home at the end of their life.
Embrace Hospice understands that these spiritual practices can, and should be, honored. We’re here to accommodate by providing professional, competent, caring, in-home service that maintains sensitivity to these values.
Care goes beyond medical support. We are prepared to and can help you and your family with the hospice and bereavement journey with sensitivity toward AAPI’s religious, spiritual, cultural, and personal beliefs. This respect extends beyond rites and rituals and into practical care. The Native Hawaiian belief that spiritual essence (mana) is in all parts of the body can, for example, influence feelings about organ donation or cremation. But awareness of this belief informs our good care for a Native Hawaiian in the end stage of life.
The AAPI population is growing. By 2050, AAPI will become nearly 10% of the total United States population. It’s important that they can get the end-of-life care they need. Our staff ensures that everyone in our care, their family, and their loved ones are treated with respect.
Some Eastern philosophies view death as part of a cycle in which a loved one’s passage serves as a reminder to celebrate the miracle of life. Our team celebrates the lives of the people we care for, and what makes each of them unique. We’re proud to join this month’s celebration of Asian and Pacific Islander American Heritage Month. We invite interested AAPI Americans to learn about our hospice and in-home services, confident their culture and traditions will be honored.